Why custom form and fit are critical to restoring function and improving outcomes in Total Knee Arthroplasty
 Knee geometry is as unique as a fingerprint, yet historical limitations in manufacturing have forced surgeons to fit highly differentiated patient anatomy to a limited range of pre-set implant sizes. Luckily, that is no longer the only option. Conformis has upended the industry paradigm with cutting-edge technology in 3D imaging and additive manufacturing to produce patient-conforming implants that match the unique anatomy of each knee, leading to smoother surgery for physicians and better outcomes for patients.
Knee geometry is as unique as a fingerprint, yet historical limitations in manufacturing have forced surgeons to fit highly differentiated patient anatomy to a limited range of pre-set implant sizes. Luckily, that is no longer the only option. Conformis has upended the industry paradigm with cutting-edge technology in 3D imaging and additive manufacturing to produce patient-conforming implants that match the unique anatomy of each knee, leading to smoother surgery for physicians and better outcomes for patients.
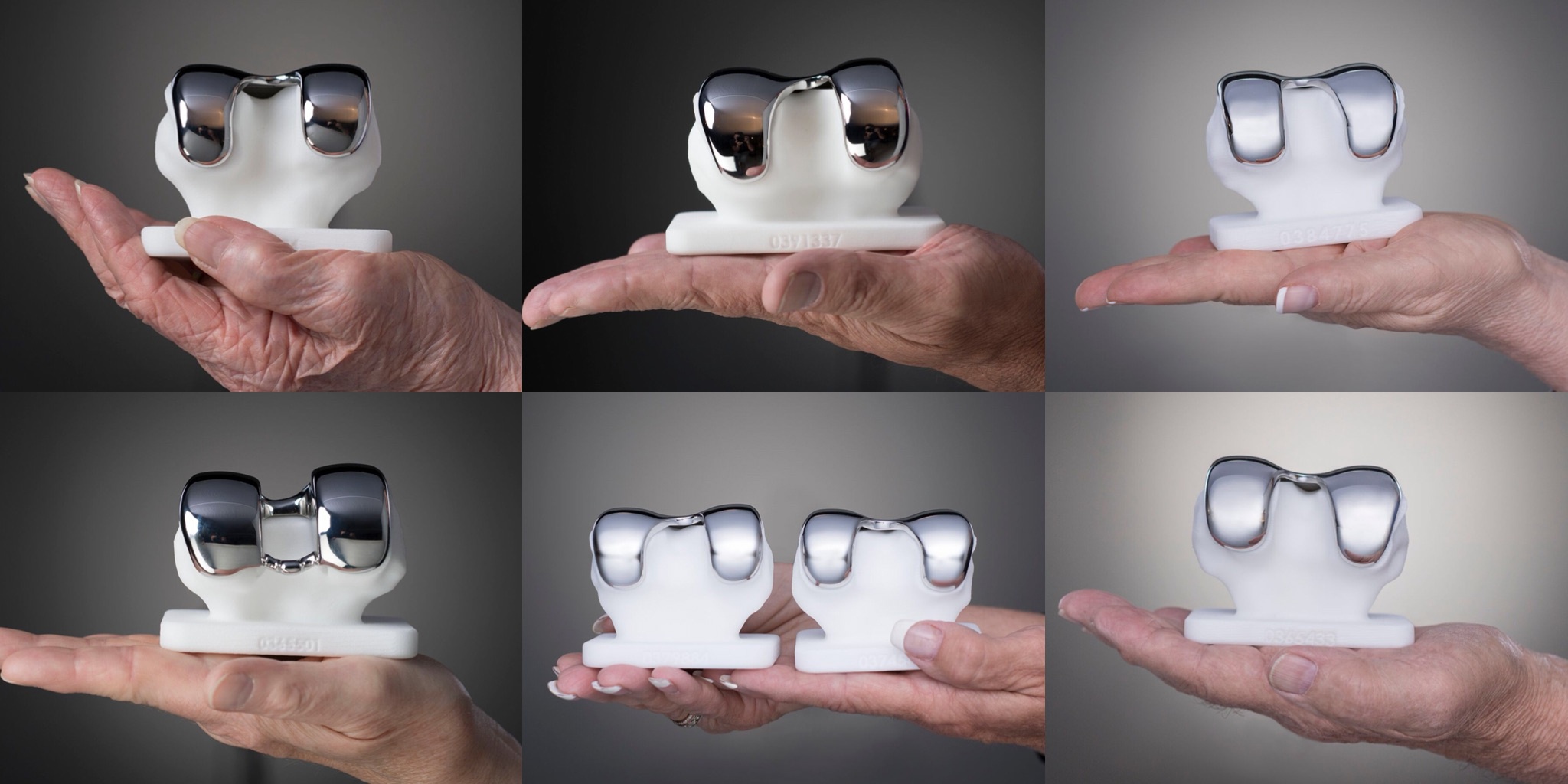
At the Conformis manufacturing facility, CAD engineers oversee automated software conversion of individual CT images into patient-specific implant designs, rows of 3D printers churn out fully disposable instruments sets, and hundreds of machines cut, mold and shape implant materials to precise, patient-specific dimensions. The result is one completely personalized kit per patient. Our obsession with personalization stems from our deeply held conviction that anatomic form plus patient-specific fit are crucial to restoring function to the joint. A more precise implant shape which better mimics native geometry allows surgeons a higher degree of control to fine-tune the procedure and deliver the best outcome for the patient.
How anatomic form leads to improved outcomes
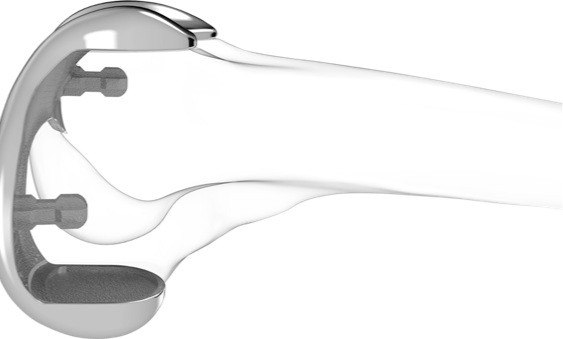
 Knee arthroplasty is often referred to as a soft tissue procedure, due to balancing that is needed in order to fit the implant to the patient. Conformis aims to take the focus away from soft tissue balancing by designing implants that respect each patient’s natural condylar shape and follow the contour of their unique anatomy.
Knee arthroplasty is often referred to as a soft tissue procedure, due to balancing that is needed in order to fit the implant to the patient. Conformis aims to take the focus away from soft tissue balancing by designing implants that respect each patient’s natural condylar shape and follow the contour of their unique anatomy.
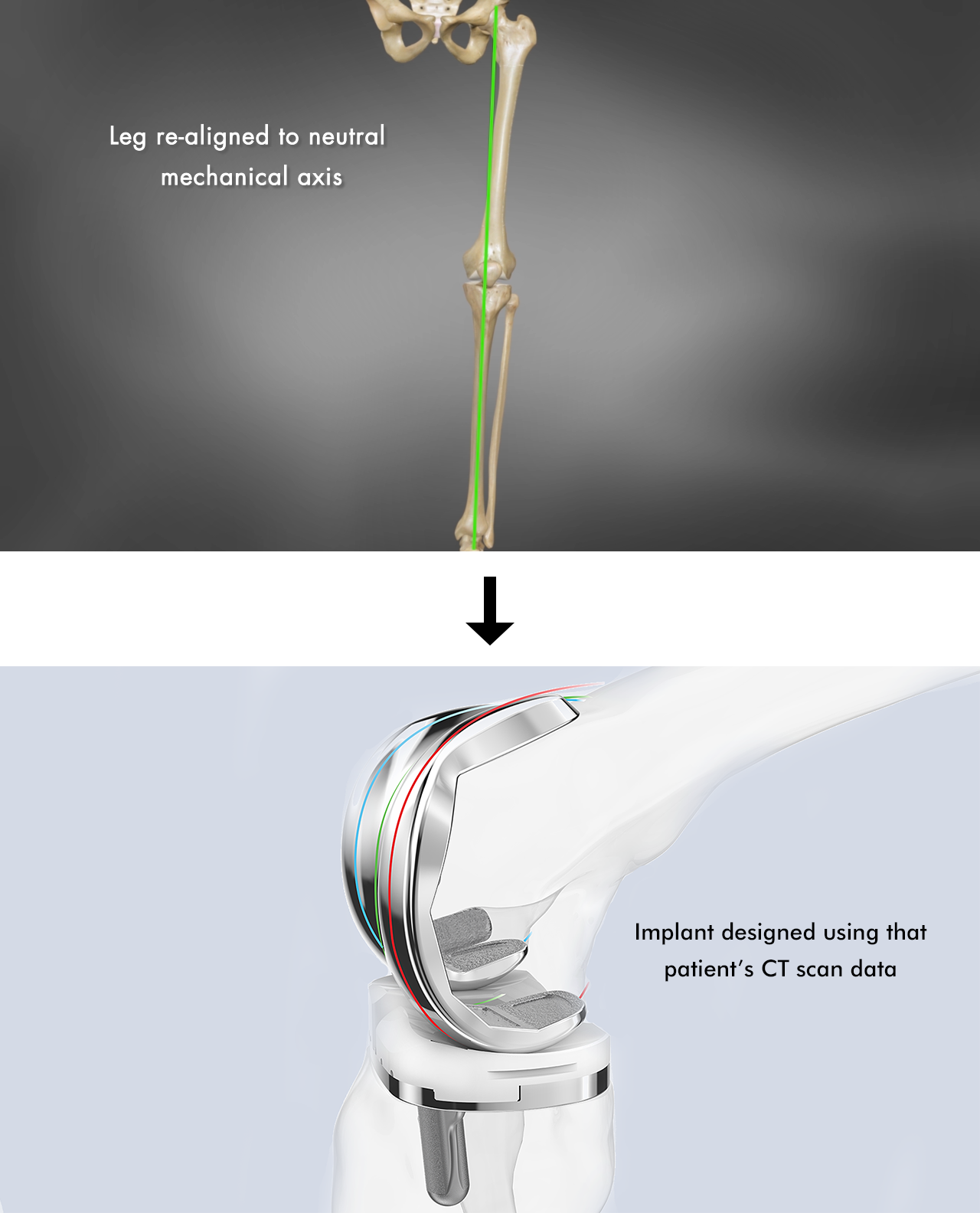
First, our propriety image-to-implant technology uses CT data to virtually align the leg to neutral mechanical axis using anatomic landmarks (center of hip, knee and ankle). Then, the software recreates the patient’s native articulating geometry by reconstructing the three independent anatomic J-curves of the patient’s medial, lateral, and patellofemoral compartments, corrected for deformity, and creating matching offset poly inserts. Hence, the shape built out on the surface of the femoral component retains patient-specific characteristics that provide stability through range of motion – the knee can now be balanced in extension, flexion, and every point in between.
The Conformis iTotal implant system puts the control to deliver a balanced knee into the hands of the surgeon through 100% patient-specific bone cuts and multiple poly insert options. The surgeon receives a pre-operative plan for each patient, called the “iView”, which provides 3D images of the bone surfaces, implant placement and operative guidance for critical cuts. The patient-conforming shape also drives kinematics, allowing femoral rollback and axial rotation to occur in a manner similar to the natural knee. Two recent studies showed more normal kinematic patterns in Conformis customized total knee replacements when compared to traditional off-the-shelf brands, including more normal rollback and axial rotation patterns, less lift-off through mid-flexioni and greater weight-bearing range of motionii.
How patient-specific fit leads to improved outcomes
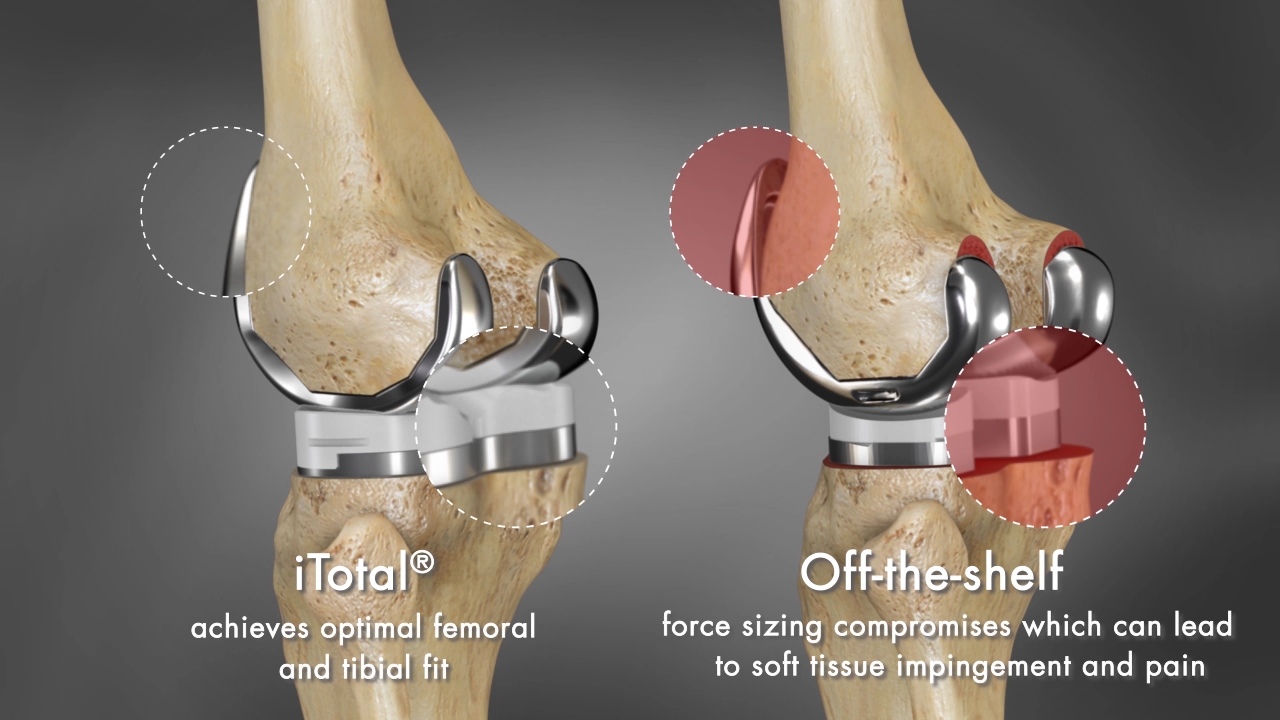 When it comes to fit, close isn’t good enough. Often, on the tibial side, surgeons are forced to compromise on either coverage or rotational alignment. One study of 120 off-the-shelf implants found that only 30% of tibial trays were aligned within 5 degrees of proper rotation.iii There is a direct correlation between internal component rotation and the severity of patellofemoral complications, including patella maltracking, subluxation, dislocation and even prosthesis failure.iv Meanwhile, sacrificing coverage for proper rotation risks problems related to implant overhang or undercoverage. Femoral overhang of >3mm has been shown to be a significant cause of residual pain in total knee replacement, affecting 40% of men and 68% of women in one study.v
When it comes to fit, close isn’t good enough. Often, on the tibial side, surgeons are forced to compromise on either coverage or rotational alignment. One study of 120 off-the-shelf implants found that only 30% of tibial trays were aligned within 5 degrees of proper rotation.iii There is a direct correlation between internal component rotation and the severity of patellofemoral complications, including patella maltracking, subluxation, dislocation and even prosthesis failure.iv Meanwhile, sacrificing coverage for proper rotation risks problems related to implant overhang or undercoverage. Femoral overhang of >3mm has been shown to be a significant cause of residual pain in total knee replacement, affecting 40% of men and 68% of women in one study.v
Since Conformis implants are based on preoperative CT scans, surgeons need not choose between coverage and rotation – coverage is maximized and proper rotational alignment is determined based on the patient anatomy, while allowing the surgeon up to 5 degrees of flexibility to dial in. Conformis implants also include a patient-specific cutout for the popliteus tendon if required, virtually eliminating the risk of pain and discomfort associated with popliteus “popping”. With a 6-cut chamfer design, the Conformis knee system offers a thinner implant without sacrificing strength and an overall 28% volumetric bone preservation advantage when compared to standard off-the-shelf implants.vi Due to broad coronal radius and coverage, Conformis implants offer high contact area with low constraint throughout the range of motion to reduce contact stress and wear.vii In short, where traditional knee arthroplasty might seem full of dichotomies, Conformis refuses to compromise.
Form, Fit and Function
Improved implant form and fit leads to improved function and outcomes. This is not a new idea; it is reflected in the ever-expanding range of implant sizes and shapes available on the market today. Since the beginning of total knee replacement, individualized anatomic implants have been considered ideal – now, modern technology has made it a reality. Conformis is the first and only company that has succeeded in commercializing individualized anatomic total knee replacements. It has been no small feat, but we have been driven by our conviction that surgeons and patients deserve something better than the limitations of off-the-shelf implants; that a more advanced implant system gives surgeons the intra-operative freedom to apply his or her expertise at a higher level. We believe that the future of successful knee arthroplasty lies in a skilled surgeon with a Conformis patient-specific implant in his or her hands.

i Zeller, Ian M., Adrija Sharma, William B. Kurtz, Mathew R. Anderle, and Richard D. Komistek. “Customized versus patient-sized cruciate retaining total knee arthroplasty: an in vivo kinematics study using mobile fluoroscopy.” The Journal of Arthroplasty 32.4 (2017): 1344-1350.
ii Zeller, IM; Ta, MD; Dessinger, GM; Kurtz, WB; Sharma, A; Komistek, RD. “In-Vivo Kinematics for Traditional and Patient-Specific Posterior Stabilized Total Knee Arthroplasty during Activities of Daily Living.” Presentation from the British Association for Surgery of the Knee meeting 2017, paper #0105
iii Martin, et al; Optimizing Tibial Coverage is Detrimental to Proper Rotational Alignment. Poster from AAHKS Annual Meeting: 2012
iv Berger, et al; Malrotation Causing Patellofemoral Complications after Total Knee Arthroplasty. Clinical Orthopaedics and Related Research; 1998, 356: 144-153
v Mahoney, et al; Overhang of the Femoral Component in Total Knee Arthroplasty: Risk Factors and Clinical Consequences. The Journal of Bone and Joint Surgery; 2010, 92: 1115-1121
vi Kurtz, William, John Slamin, and Scott Doody. “Bone Preservation in a Novel Patient Specific Total Knee Replacement.” Reconstructive Review 6.1 (2016): 23-29.
vii Data on file.
Centro risorse per i chirurghi
Centro risorse per i chirurghiMedical Education
Medical EducationContattaci: international@conformis.com